Welcome to our health education library. The information shared below is provided to you as an educational and informational source only and is not intended to replace a medical examination or consultation, or medical advice given to you by a physician or medical professional.

Vasectomy is a simple, safe procedure that makes a man sterile (unable to father a child). It is the most effective birth control method for men.
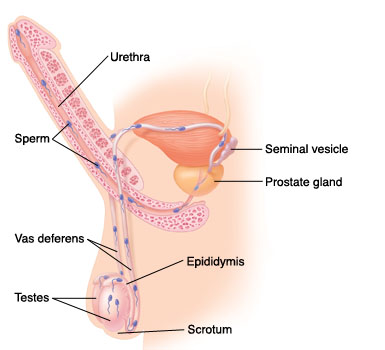
Your Reproductive System
For pregnancy to occur, a man’s sperm (male reproductive cells) must join with a woman’s egg. To understand how a vasectomy works, you need to know how sperm are produced, stored, and released by the body.
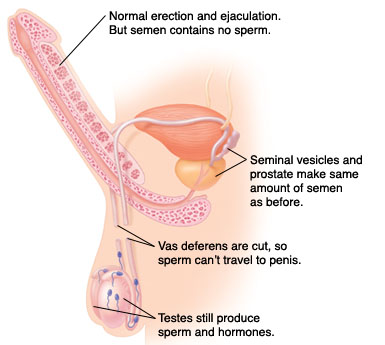
How a Vasectomy Works
During the procedure, the two vas deferens are cut and sealed off. This prevents sperm from traveling from the testes to the penis. It is the only change in your reproductive system. The testes still produce sperm. But since the sperm have nowhere to go, they die and are absorbed by your body. Only a very small amount of semen is made up of sperm. So after a vasectomy, your semen won’t look or feel any different.
Keep In Mind
After a vasectomy, some active sperm still remain in the reproductive system. It will take about 3 months and numerous ejaculations before the semen is completely free of sperm. Until then, you’ll need to use another form of birth control.
 |  |
A vasectomy is an outpatient (same day) procedure. It can be done in a doctor’s office, clinic, or hospital. Before your vasectomy will be performed, you’ll be asked to read and sign a consent form. This form states you’re aware of the possible risks and complications and understand that the procedure, though usually successful, is not guaranteed to make you sterile. Be sure that you have all your questions answered before signing this form. After the procedure, if you have any of the following or other symptoms you’re concerned about, call your doctor.
Possible Risks and Complications of Vasectomy
Vasectomy is a safe procedure. But it does have risks, including bleeding and infection. You may also have any of the following after surgery:
The no-scalpel procedure is similar to a traditional vasectomy in many respects, but it’s done without incisions or stitches. This generally results in faster healing.
Talk to your health care provider on how to prepare for the procedure, and about any risks and complications.
During the Procedure
After the Procedure
If you’ve been given medications to help you relax, you’ll need to have someone drive you home. The local anesthetic begins to wear off after an hour or so. Any discomfort you feel is usually very mild. If you need it, a pain reliever may help.
During Your Healing
Recovery time after a no-scalpel vasectomy is usually less than after a traditional vasectomy. Once you’re home, you can do several things to aid your recovery:
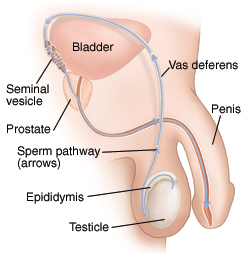
Each of a man’s testicles makes sperm (male reproductive cells). Sperm travel from the testicles to the penis through one of two tubes called the vas deferens. On the way, sperm mix with other fluids to form semen, which leaves the body during ejaculation. During a vasectomy, each vas deferens is cut, blocking sperm from leaving the body. This makes you sterile (unable to make a woman pregnant). A vasectomy can sometimes be reversed, restoring the flow of sperm out of the body.
How the Procedure Works
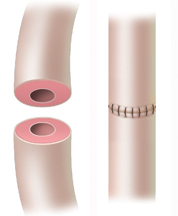
During a vasectomy reversal, the two cut ends of the vas deferens are stitched back together. With the sperm pathways restored, sperm can once again travel through the vas deferens and leave the body during ejaculation. You may then be able to father a child.
Preparing for the Procedure
You will be given instructions to prepare for the vasectomy reversal. Tell your healthcare provider about any medications you take, including aspirin. You may be asked to stop taking some or all of these. On the day of your procedure, bring clean cotton briefs or an athletic supporter with you.
During the Procedure
You’ll receive medication to keep you comfortable. You may be awake and relaxed during the procedure. Or, you may be completely asleep. Once the medication takes effect:
After the Procedure
You may need to stay in the hospital for several hours. When it’s time to go home, have an adult family member or friend drive you. Once you’re home:
Possible Risks and Complications
 |  |
Vasectomy is an outpatient (same day) procedure. It can be done in a doctor’s office, clinic, or hospital. Your doctor will talk with you about preparing for surgery. He or she will also discuss the possible risks and complications with you. After the procedure, follow all your doctor’s advice for recovery.
Preparing for Surgery
Your doctor will talk with you about getting ready for surgery. You may be asked to do the following:
During Surgery
The entire procedure usually lasts less than 30 minutes.
Recovering at Home
For about a week, your scrotum may look bruised and slightly swollen. You may also have a small amount of bloody discharge from the incision. This is normal.
To help make your recovery more comfortable, follow the tips below.
Sex After Vasectomy
Vasectomy doesn’t change your sexual function. So when you start having sex again, it should feel the same as before. A vasectomy also shouldn’t affect your relationship with your partner. It’s important to remember, though, that you won’t become sterile right away. It will take time before you can have sex without the need for birth control.
Call your doctor if you notice any of the following after surgery:
An intravenous pyelogram (IVP) is an x-ray exam of your urinary tract (kidneys, ureters, and bladder). This test can help find stones or other problems with your urinary tract.
Before Your Test
During Your Test
For your safety, the technologist needs to know about any of the following:
Your Test Results
Your doctor will discuss the test results with you during a follow-up visit or over the phone.
Passing a kidney stone can be very painful. Shock wave lithotripsy is a treatment that helps by breaking the kidney stone into smaller pieces that are easier to pass. This treatment is also called extracorporeal shock wave lithotripsy (ESWL). Lithotripsy takes about an hour. It’s done in a hospital, lithotripsy center, or mobile lithotripsy van. You will likely go home the same day.
During the Procedure
After the Procedure
Passing the Stone
It can take a day to several weeks for the pieces of stone to leave your body. Drink plenty of liquids to help flush your system. During this time:
Possible Risks and Complications
Call Your Doctor If You Have:
A ureteral stent is a soft plastic tube with holes in it. It’s temporarily inserted into a ureter to help drain urine into the bladder. One end goes in the kidney. The other end goes in the bladder. A coil on each end holds the stent in place. The stent can’t be seen from outside the body. It shouldn’t interfere with your normal routine. Your stent will be put in by a urologist (doctor trained in treating the urinary tract) or another specialist. The procedure is done in a hospital or surgery center. You’ll likely go home the same day.
When Is a Ureteral Stent Used?
A ureteral stent may be used:
Before the Procedure
Your doctor will give you instructions to prepare for the procedure. X-rays or other imaging tests of your kidneys and ureters may be done beforehand.
During the Procedure
While You Have a Stent
How Long Will You Need a Stent?
The stent is often taken out after the blockage in the ureter is treated or the ureter has healed. This may take 1-2 weeks, or longer. If a stent is needed for a long time, it may need to be changed every few months.
Call Your Doctor If:
The study may be done in the doctor’s office, a clinic, or a hospital. Depending on which tests are being done, the study may take up to an hour or more. The tests are generally painless, so you don’t need sedating medication.
Tests That May Be Done
Uroflowmetry measures the amount and speed of urine you void from your bladder. You urinate into a funnel attached to a computer that records your urine flow over time. The amount of urine left in your bladder after you void may also be measured immediately after this test.
Cystometry evaluates how much the bladder can hold, how strong the bladder muscle is, and how well the signals work that tell you when your bladder is full. Through a catheter, your bladder is filled with sterile water or saline solution. You’re asked to report any sensations you feel and whether they’re similar to symptoms you’ve felt at home. You may be asked to cough, stand and walk, or bear down during this test.
Electromyogram helps evaluate the muscle contractions that control urination. Electrode patches or wires may be placed near the rectum or urethra to make the recording. You may be asked to try to tighten or relax your sphincter muscles during this test.
Pressure flow study measures the pressure and flow of urine out of your bladder. It is often performed after cystometry. You’re asked to urinate while a probe in the urethra measures pressures.
Video cystourethrography takes video pictures of urine flow through the urinary tract. It can help identify blockages or other problems. The bladder is filled with an x-ray contrast fluid, then x-ray video pictures are taken as the fluid is urinated out.
Getting Your Results
When the study is finished, you’ll get dressed and return to the consultation room. Test results may be available soon after the study is finished, or you may return to your doctor’s office in a few days for your results. Your doctor can talk with you about the study report and your options.
A urodynamics study is a series of tests that gives your doctor a detailed look at the function of your bladder and urethra. These tests can help your doctor evaluate any problems you may be having with storing urine or voiding (eliminating) urine from your body.
Understanding the Lower Urinary Tract
The lower part of the urinary tract includes the bladder (which stores urine until you’re ready to release it) and the urethra (the canal that carries urine from the bladder out of the body). Signals from the brain tell the sphincter(muscles around the opening of the bladder) when to relax and the bladder when to contract to let urine flow out of the body.
Why You Need a Urodynamics Study
Possible problems that you may have with storing or voiding urine include the following:
Preparing for the Study
Tell your doctor which medications you’re taking, and ask whether you should stop them before the study. You may be asked to keep a diary of your urination habits for a few days before the study. This diary can be a helpful part of your evaluation. Ask whether you need to arrive for the study with a full bladder.
Cystectomy is the surgical removal of the entire bladder. This surgery may be suggested in certain cases of bladder cancer, especially high-grade, high-stage cancer. Your doctor can discuss the risks and benefits of cystectomy with you. If you decide to have surgery, the surgeon can explain the procedure and answer your questions.
Preparing for Surgery
You’ll be given instructions on how to prepare for your surgery. These may include the following:
Removing the Bladder
The surgery is done in the hospital. It generally takes 4-6 hours, but can take longer depending on the situation. You’ll be given general anesthesia so you sleep throughout the procedure. An incision is made near your bellybutton. The area around your bladder is examined to see if the cancer has spread. If it has, the procedure may not be continued. If the cancer is only in the bladder, the bladder is removed. In case cancer cells have already spread, other organs near the bladder are often removed as well.
Creating a New Path for Urine
When the bladder is removed, another way to store and release urine is needed. This often means making a new opening for urine to travel out of the body. This procedure is called a urostomy. Your doctor will explain this procedure to you.
Risks and Possible Complications
Cystoscopy is a procedure that lets your doctor look directly inside your urethra and bladder. It can be used to:
Based on the findings, your doctor may recommend other tests or treatments.
What Is a Cystoscope?
A cystoscope is a telescope-like instrument that contains lenses and fiberoptics (small glass wires that make bright light). The cystoscope may be straight and rigid, or flexible to bend around curves in the urethra. The doctor may look directly into the cystoscope, or project the image onto a monitor.
Getting Ready
To prepare, stop taking any medications as instructed. Ask whether you should avoid eating or drinking anything after midnight before the procedure. Follow any other instructions your doctor gives you.
The Procedure
Cystoscopy is done in the doctor’s office or hospital. The doctor and sometimes a nurse are present during the procedure. It takes only a few minutes, longer if a biopsy, x-ray, or treatment needs to be done. During the procedure:
After the Procedure
If you had a sedative, general anesthesia, or spinal anesthesia, you must have someone drive you home. Once you’re home:
Tell your doctor before the exam if you:
Cystography (also called retrograde cystography) is an exam of the bladder using x-rays. This test is done by a radiologist, a doctor who specializes in the use of x-ray imaging to diagnose and treat health conditions. During a cystography, the bladder is filled with a special contrast medium(x-ray dye) or radioactive medium (radionuclide). This medium ensures more detailed x-ray pictures.
Why Cystography Is Done
A cystography can help diagnose such bladder problems as:
Preparing for the Procedure
During the Procedure
After the Procedure
Potential Risks and Complications Include
Call your doctor after the procedure if you notice:
Ultrasound is an imaging test. It uses sound waves to form pictures of your organs that appear on a screen. Transrectal ultrasound uses a special probe that is placed directly into the rectum. This test lets your doctor assess the prostate gland, which is in front of your rectum. During the test, tissue samples (biopsy) may also be taken.
Preparing for Your Test
During Your Test
After the Test
Before leaving, you may need to wait for a short time while the images are reviewed. In most cases, you can go back to your normal routine after the test. If you had a biopsy, you may notice some blood in your urine or stool for a day or so. This is normal. Your doctor will let you know when the results of your test are ready. Be aware that although the sonographer can answer questions about the test, only a doctor can explain the results.
Call your doctor if:
Circumcision is a procedure to remove the foreskin, the loose fold of skin that covers the head of the penis. You may have a condition that requires circumcision. Or, you may want to be circumcised for personal reasons. Either way, you will want to know what to expect. Read on to learn more about adult circumcision and how it’s done.
Before the Procedure
Tell your doctor about all medications you take and any allergies you have. Cream to numb the skin of the penis may be applied 30 to 60 minutes before the procedure. Also, there will be some swelling and soreness after the procedure, so arrange for an adult family member or friend to drive you home.
During the Procedure
After the Procedure
You will be taken to a recovery area where you’ll recover from the anesthesia. Nurses will check on you as you rest. They can also give you pain medication if needed. Your doctor will tell you when it’s okay for you to go home. This will be the same day. When you dress to go home, wear snug-fitting, brief-style underwear. This will help hold your bandage in place. You will also be given care instructions for when you return home.
What to Expect
Caring for Your Penis
Follow-Up
Make a follow-up appointment as directed by our staff.
Call the healthcare provider right away if you have any of the following:
To help treat stress urinary incontinence (SUI), your surgeon may perform a procedure called retropubic suspension. This surgery is done laparoscopically-that means through small incisions in the belly. During the surgery, sutures are used to firmly support the pelvic organs and help prevent urine leakage. Your surgery will take about 2 hour(s). You will be asked to do some things at home to prepare for surgery. Below are guidelines to help you get ready. If you have any questions, call your nurse or doctor.
The Weeks Before Surgery
The Night Before Surgery
The Day of Surgery
Arrive at the hospital a few hours before surgery as directed. Have someone drive you there who can also stay during the surgery, and drive you home. At the hospital, your temperature and blood pressure will be taken. In some cases, tests may be done. Then, you will receive one or more IV (intravenous) lines. These lines give you fluids and medications before, during, and after surgery. Some of your pubic hair may be removed. Tight stockings may be put on your legs to help prevent blood clots.
About Anesthesia
To keep you pain-free during surgery, you’ll receive anesthesia. General anesthesia allows you to sleep. Regional anesthesia numbs the lower part of your body. Local anesthesia numbs the area that will be operated on. Before surgery, you’ll meet with the anesthesiologist or nurse anesthetist. He or she can tell you what kind of anesthesia you will receive and answer questions you may have.
During the Procedure
Risks and Complications
The risks and complications of this procedure may include:
To help treat stress urinary incontinence (SUI), your surgeon may perform a procedure called retropubic suspension. It is done by making an incision in the lower part of your belly (abdomen). During this surgery, the surgeon puts sutures (stitches) through the tissue next to the vagina to help support the urethra and bladder firmly in place. This helps keep the urethra closed to prevent urine leakage. Your surgery will take about 2 hour(s). You will be asked to do some things at home to prepare for surgery. Below are guidelines to help you get ready. If you have any questions, call your nurse or doctor.
The Weeks Before Surgery
The Night Before Surgery
The Day of Surgery
Arrive at the hospital a few hours before surgery as directed. Have someone drive you there who can also stay during the surgery, and drive you home. At the hospital, your temperature and blood pressure will be taken. In some cases, tests may be done. Then, you will receive one or more IV (intravenous) lines. These lines give you fluids and medications before, during, and after surgery. Some of your pubic hair may be removed. Tight stockings may be put on your legs to help prevent blood clots.
About Anesthesia
To keep you pain-free during surgery, you’ll receive anesthesia. General anesthesia allows you to sleep. Regional anesthesia numbs the lower part of your body. Local anesthesia numbs the area that will be operated on. Before surgery, you’ll meet with the anesthesiologist or nurse anesthetist. He or she can tell you what kind of anesthesia you will receive and answer questions you may have.
During the Procedure
Risks and Complications
The risks and complications of this procedure may include:
To help treat stress urinary incontinence (SUI), your surgeon may perform a procedure called pubovaginal sling surgery. A “sling” of tissue is placed like a hammock under the bladder and urethra. The sling helps support the bladder and urethra firmly in place. This helps keep the urethra closed to prevent urine leakage. Your surgery will take about 2 hour(s). You will be asked to do some things at home to prepare for surgery. Below are guidelines to help you get ready. If you have any questions, call your nurse or doctor.
The Weeks Before Surgery
The Night Before Surgery
The Day of Surgery
Arrive at the hospital a few hours before surgery as directed. Have someone drive you there who can also stay during the surgery, and drive you home. At the hospital, your temperature and blood pressure will be taken. In some cases, tests may be done. Then, you will receive one or more IV (intravenous) lines. These lines give you fluids and medications before, during, and after surgery. Some of your pubic hair may be removed. Tight stockings may be put on your legs to help prevent blood clots.
About Anesthesia
To keep you pain-free during surgery, you’ll receive anesthesia. General anesthesia allows you to sleep. Regional anesthesia numbs the lower part of your body. Local anesthesia numbs the area that will be operated on. Before surgery, you’ll meet with the anesthesiologist or nurse anesthetist. He or she can tell you what kind of anesthesia you will receive and answer questions you may have.
During the Procedure
Risks and Complications
The risks and complications of this procedure may include:
To help treat stress urinary incontinence (SUI), your surgeon may perform a procedure called tension-free vaginal sling surgery. A “sling” of tissue is placed under the urethra. The sling (tape) is made from synthetic (manmade) material. When the tension of the tape is adjusted, urine should no longer leak. Your surgery will take about 60 minutes. You will be asked to do some things at home to prepare for surgery. Below are guidelines to help you get ready. If you have any questions, call your nurse or doctor.
The Weeks Before Surgery
The Night Before Surgery
The Day of Surgery
Arrive at the hospital a few hours before surgery as directed. Have someone drive you there who can also stay during the surgery, and drive you home. At the hospital, your temperature and blood pressure will be taken. In some cases, tests may be done. Then, you will receive one or more IV (intravenous) lines. These lines give you fluids and medications before, during, and after surgery. Some of your pubic hair may be removed. Tight stockings may be put on your legs to help prevent blood clots.
About Anesthesia
To keep you pain-free during surgery, you’ll receive anesthesia. General anesthesia allows you to sleep. Local anesthesia numbs the area that will be operated on. Before surgery, you’ll meet with the anesthesiologist or nurse anesthetist. He or she can tell you what kind of anesthesia you will receive and answer questions you may have.
During the Procedure
Risks and Complications
The risks and complications of this procedure may include:
After a urostomy, you’ll have to care for your stoma and the skin around it (peristomal skin). You must keep the stoma clean and protect the peristomal skin from moisture and urine. This is to prevent skin problems and odor.
Checking the Stoma
Cleaning the Stoma
When you change your pouch, be sure to clean the stoma and the skin around it. Do this using warm water and a soft washcloth. Water does not harm the stoma.
Protect the Skin Around the Stoma
For the pouch to stick well, the peristomal skin needs to be dry and smooth. If the skin is moist or uneven, the pouch is more likely to leak. And any urine that leaks out of the pouch can pool on your skin. This can irritate the skin. Urine that leaks from the pouch can also cause odor or be absorbed by your clothes. You can help prevent these problems by following these steps:
Call Your WOC Nurse or Other Healthcare Provider If:
You’ve just had a urostomy. As part of your surgery, a small opening (stoma) was made on the abdomen. Urine and mucus drain from the stoma into a disposable pouch. You’ll be shown how to change your pouch before you leave the hospital. Plan to replace your pouch every few days. And change it early in the morning, when your urine output is less. To change your pouch, follow the steps below.
How to Change Your Pouch
Step 1: Prepare the new pouch.
Step 2: Remove the used pouch.
Step 3: Clean around the stoma.
Step 4: Put on the new pouch.
Call Your WOC Nurse or Other Healthcare Provider If:
You’ve just had a urostomy. As part of your surgery, a small opening (stoma) was made on the abdomen. Urine and mucus drain from the stoma into a disposable pouch. You’ll need to empty your pouch regularly when it gets to be about one-third full. The pouch is likely to become this full every 2 to 3 hours. Emptying your pouch keeps the pouch from bulging under your clothes. It also helps prevent leakage and odor. To empty your pouch, follow the steps below.
How to Empty Your Pouch
Step 1: Empty the pouch.
Step 2: Close the pouch drain.
You’ve just had a urostomy to provide a new way for urine to drain from your body. Follow the tips on this sheet to learn how to maintain your health and help prevent problems.
A Few Words on Diet
Drinking Plenty of Water
Taking a Shower or Bath
When You Have a Checkup
If You Have Symptoms of a Urinary Tract Infection
Call your WOC nurse or other healthcare provider if you have any of the following symptoms of a urinary tract infection:
Getting Support
Adjusting to a urostomy takes time. But your family and friends can help you. Your surgeon, WOC nurse, and other healthcare providers are there to answer your questions, too. And they can help you find a support group. This is a group of people who share similar concerns or problems. You can also contact the organizations listed below:
You’ve just had a urostomy. As part of your surgery, a small opening (stoma) was made on the abdomen. Taking good care of the skin around the stoma is very important to prevent skin problems. If a problem does occur, you need to know what to do. Listed below are some of the most common skin problems and steps you can take to manage them. If any of these problems lasts more than a week, call your WOC nurse or other healthcare provider. If your pouch leaks, use a measuring guide to check that the pouch opening is the correct size.
Common Skin Problems
After a urostomy, urine drains into a disposable pouch. The pouch sticks to the skin around the stoma. An adhesive skin barrier holds the pouch in place. This barrier also protects the skin and prevents leakage. Most pouches are made of lightweight, odorproof plastic and lie flat against the body.
Types of Pouches
There are many styles of pouches. Your WOC nurse or other healthcare provider will help you select the one that’s best for you. The skin barrier has to fit around the stoma without touching it. The barrier must stick well to prevent leakage or odor from the pouch.
One-Piece Drainable Pouch
Two-Piece Drainable Pouch
Sizing the Stoma Opening
For the pouch to fit around the stoma, the opening of the skin barrier must be the right size. Some openings are precut, and others must be measured and cut. To find the correct size for your stoma, use a measuring guide. Most pouches come with a guide in the box. Your healthcare provider may also give you one.
Pouch Accessories
You can buy other stoma care products through special catalogs, at medical supply stores, on the Internet, and at some drugstores.
You’ve just had a urostomy. As part of your surgery, a small opening (stoma) was made on the abdomen. Urine and mucus drain from the stoma into a disposable pouch. A night drainage system can be attached to the pouch before you go to bed. This system then collects and stores urine. That way, you can sleep all night without getting up to empty the pouch.
Parts of a Night Drainage System
The parts of a night drainage system are shown above. Some people use a catheter (tube) drainage bag to collect and store the urine overnight. Talk with your WOC nurse or other healthcare provider about what will work best for you.
Setting Up the Night Drainage System
There are several types of night drainage systems. Whichever type you chose, you need to set up the system before connecting it to the pouch. Be sure to do the following:
At Night
The pouch should be about one-fourth full when you attach the drainage system to it at night. This will help urine flow into the tubing from the pouch. To attach the system to your pouch:
In the Morning
To detach the night drainage system from the pouch each morning:
Cleaning the System
Clean the night drainage system every 2 to 3 days. Follow these steps:
Urostomy is surgery that provides a new way for the body to release urine (waste fluid). It is done when the bladder is diseased or damaged. During the surgery, the surgeon brings part of the urinary tract or some of the digestive tract through the abdominal wall. Urostomy can be done in any of the ways described below. In each case, a small opening (stoma) is made on the abdomen. This allows urine and mucus to pass out of the body.
The Urinary Tract
This tract rids the body of urine and is made up of many parts. They include two kidneys, two ureters, the bladder, and the urethra.
Common Types of Urostomies
These include:
The Stoma
The stoma is an opening on the abdomen through which urine and mucus can pass. It is made by bringing the end of the ileum, the colon, or one or both ureters through the abdominal wall. This end is then turned back on itself, like a cuff.
Serving people of all ages from Shawano to Oshkosh. Please contact our Main Office in Neenah, WI for more information, (920) 886-8979 or (877) 897-7747.
Fax: (920) 886-2225.
WIU’s New London location is relocating.
Check us out at 1370 N Shawano St. Suite A, New London, WI 54961-7943